My Family Member Developed a Bedsore:
Should I Call a Bed Sore Lawyer?
When a patient is neglected, deep bed sores can develop on their skin. Bed sores are preventable wounds that cause unnecessary pain and suffering. There is no excuse for allowing a bedsore to develop inside a facility. These pressure wound injuries generally develop from patient neglect.
At Senior Justice Law Firm, our bed sore attorneys focus on cases involving bedsore litigation. The majority of our caseload involves bed sores. Let our decades of experience and narrow focus guide you on your journey to justice.
If your loved one developed bedsores inside a nursing home, an assisted living facility, or hospital, call our bed sore lawyers now, toll-free, at 1-888-375-9998.
The consultation is free and we never require an out of pocket payment from you.
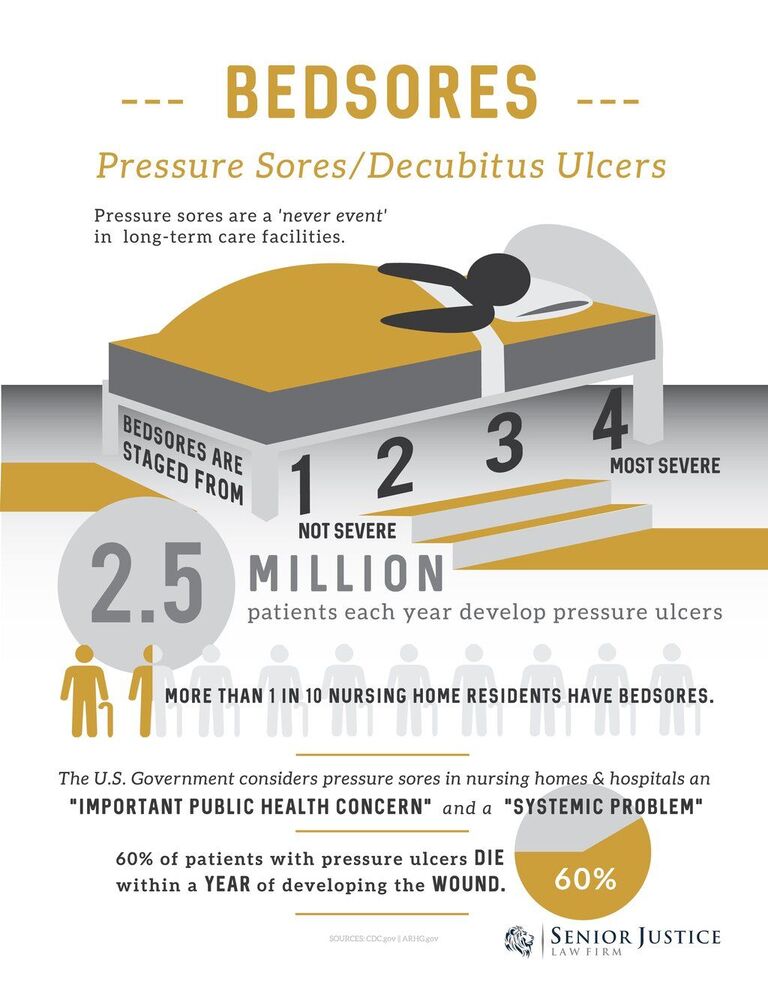
Pressure ulcers are a “never event” in hospitals and nursing homes, as per Medicare guidelines. This means they should never occur.
Senior Justice Law Firm specializes in patient neglect cases against negligent nursing homes, assisted living facilities and hospitals. This is all we do. Bed sore lawsuits are the most common injury claim we handle. Let our firm help your family seek justice today.
Attorneys Narrowly Focused on Litigating Bed Sore Injury Claims
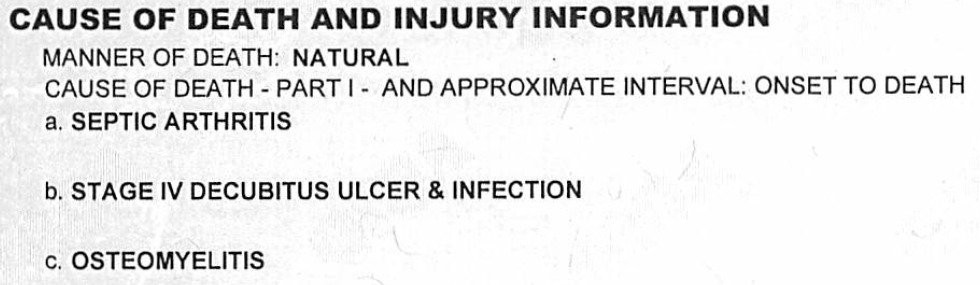
Bedsores, also called pressure sores or decubitus ulcers, frequently occur in nursing homes and hospitals as a result of nursing negligence. Bed sores are not an acceptable part of a hospitalization or nursing home residency. Untreated bed sores can result in sepsis, osteomyelitis and a whole host of other health issues, including wrongful death.
If your loved one developed bedsores inside a nursing home, assisted living facility, or hospital, report the incident immediately.
Call us now at 1-888-375-9998 or use the live chat feature to speak with one of our bed sore lawyers about your legal options.
Can I File a Lawsuit if my Parent Has Bed Sores?
Yes, you can file a bed sore lawsuit against the at-fault nursing home. A bed sore lawsuit secures compensation for your family, but also leads to facility changes and better resident care.
What differentiates bedsores from many other types of injuries in nursing homes is that bedsores are generally preventable. It is entirely possible to avoid having residents develop bedsores. This is true even in bedridden patients. All that has to be done is repositioning high risk patients while they lie in bed or in a wheelchair. This repositioning is the job of facility nurses.
Unfortunately, as nursing homes continue to push the limits on maximizing profits and minimizing expenses, more and more facilities are cutting staff to save money. Further, untrained or unqualified staff are being hired in order to pinch pennies and make nursing homes more money. This means that residents are not attended to as often as they may require, which is critical in the prevention of bedsores. This is the reason that nursing homes are at fault for pressure ulcers developed during a patient’s residency. And sadly, it is usually a profits-before-people business decision made by the corporation that is the root cause of residents developing skin breakdown.
Less than 10% of elder abuse is reported, which means that facilities housing residents with bedsores do not typically receive the disciplinary measures they need in order to amend their practices. This is part of why a bed sore lawsuit can have further-reaching benefits than just compensation for your family.
Bed sore lawsuits can catalyze change, draw attention to neglectful facility practices, improve care, and ensure that this kind of harm does not happen again. These kinds of bed sore cases do much more than just put money and compensation in your pocket.
What are my Legal Rights if a Loved One Has Bed Sores?

Many problems can arise as part of living in an assisted living facility or nursing home. Older people tend to struggle with feelings of isolation, coping with their new living circumstances, and overcoming new health challenges as they continue to age. However, one type of injury that is usually avoidable is a bed sore. If someone you love developed a bed sore—also called a pressure ulcer—you may hear a variety of explanations from the nursing home. Understand that bed sores are never acceptable, and they are never “a normal part” of life in an assisted care facility. Each nursing home has a responsibility to prevent these injuries—because they are preventable. Failure to do so can result in liability on the part of the nursing home.
When you learn your family member has developed a bedsore in a facility, take action right away. Any pressure sores that you have noticed on your family member should be shown to the doctor and head nurse as soon as possible. Document the bed sore with pictures and create a list of the nurses and doctors you have spoken to about the wound. If your loved one develops bedsores inside a hospital, assisted living, or nursing home, you should seek legal advice from one of our bed sore attorneys.
Medical facilities should be — and can be — held responsible for these preventable and horrendous wounds. The law provides for an avenue of recovery through the civil justice system. This is called a bed sore neglect lawsuit, and this claim can be filed against the negligent nursing home or hospital where the bedsore developed.
How Do Bed Sores Form in Nursing Homes?

Lack of movement and improper hygiene are major factors in developing bedsores. Pressure sores result from restricted blood flow in a particular area — usually the heels, buttocks, back and head. However, compromised blood flow does not excuse bed sores.
When an at-risk patient cannot move in bed on their own, the nursing home or hospital nurses must reposition the patient every two hours to offload pressure and prevent bedsores. If a patient is not regularly shifted around so that their body weight is distributed every few hours, these sores can begin to develop at the tailbone area, as well as the shoulder blades, heels, and surrounding the knees, as well as other locations.
If the facility staff is not repositioning every two hours, this is an example of nursing neglect. Federal laws are in place to protect patients from this carelessness. However, bedsores are still rampant throughout long-term care facilities, usually due to understaffed and overworked nurses. If a patient is left in their own urine, further underlying infections can result. The deteriorating skin can be permanently damaged.
Regular movement of patients at scheduled times (at least every two hours) and properly checking to make sure that clothing and bedding are dry are the responsibility of the nursing home or hospital. If the facility is doing an adequate job of hiring and training personnel, these routine patient care techniques should be in place. The standard of care requires that at-risk patients be turned every two hours by staff. The use of cushions, special pillows, air mattresses and other items to reduce skin pressure should be done regularly for non-mobile patients.
Bedsores, Pressure Sores and Decubitus Ulcers
5 Fast Facts About Facility-Acquired Bed Sores
- All nursing homes are required to keep track of any bedsores and skin degradation that appear in their facilities. If your loved one’s bedsore was not documented or reported in a timely manner, that is a problem for the facility.
- Health insurers will typically not reimburse a facility for the medical costs associated with treating an inhouse acquired bedsore, because these ulcers are preventable. This can lead to facilities being unwilling to provide care, because it comes at their own expense.
- The most effective treatment of bed sores is preventing the wounds from developing. A simple turning and repositioning schedule can eliminate the threat of skin breakdown.
- More than half of all patients who develop a bedsore pass away within one year of its development.
- The most common cause of death via bedsore is infection; sepsis (blood infection) and osteomyelits (bone infection).
How do Bed Sores get Infected?
Untreated decubitus ulcers are very serious and can lead to severe infection. Our bed sore attorneys commonly see the following infections due to pressure wounds:
- Osteomyelitis
- Sepsis
- E. Coli
- Cellulitis
- Septic arthritis
- Staphylococcus aureus
- Proteus mirabilis
- Pseudomonas aeruginosa
- MRSA
What Does Having a Bedsore Feel Like?
If you have never encountered a bed sore before, you may be unsure of whether it is even something that is worth “making a fuss” about. However, victims describe bedsores as debilitating. What starts out as mild irritation and discomfort can quickly evolve into agony that prevents the patient from ever getting comfortable. At the same time, these wounds typically become infected, presenting a new set of problems, downstream medical treatment, and pain. The infection can cause the skin in and around the ulcer to become necrotic (or, in other words, to die), and if the infection proceeds too deep or too much damage is done to the skin and surrounding structures, the patient can even die from a bedsore.
After years of representing bedsore victims, our bed sore lawyers have spoken with many victims of painful decubiti. Patients have described a painful, infected bedsore as absolute misery.
The underlying wound infection can also profoundly change a patient’s life. In some cases, the pressure wound can even be deadly.
These pressure injuries are not to be taken lightly, and are far more serious than rashes or surface level cuts.
What are the Stages of Bed Sores?

Bedsore photos are shocking and revolting. Even with decades of combined experience handling these kinds of claims, our bed sore lawyers are still horrified at seeing photographs of the wounds.
Bedsore pictures usually show a gaping hole in the skin, typically on the backside (sacrum) or the heels. They are painful, unsightly and can lead to deadly infections such as sepsis or MRSA.
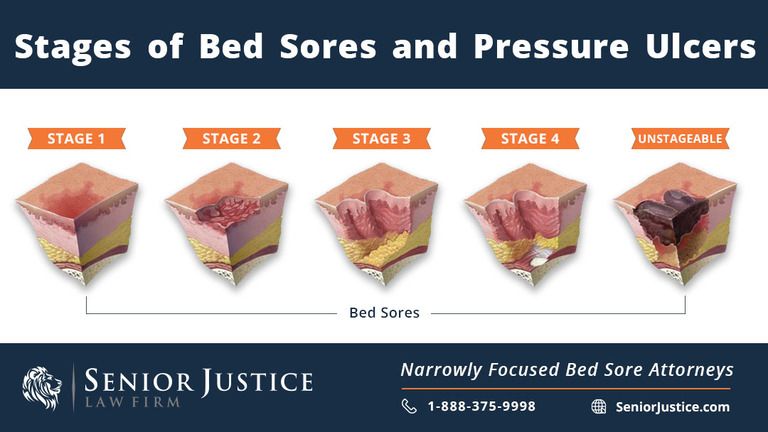
Bedsores are staged based on severity from Stage 1 to Stage 4.
Types of Bed Sores
What is a Stage 1 Pressure Sore?
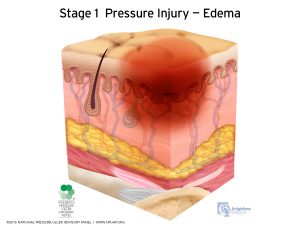
A Stage 1 bedsore is a smaller red spot. The skin is still intact, but there is a reddened area, like a rash.
This kind of wound may be painful, but if the pressure injury is caught and treated before deteriorating, there is not much damage done.
Litigation does not usually arise out of Stage 1 ulcers since they are minimal and do not pose a large health risk.
What is a Stage 2 Bed Sore?
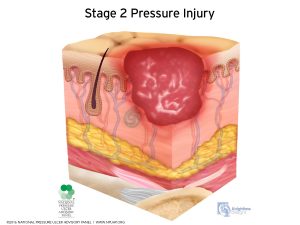
At Stage 2, a pressure ulcer now opens up and has exposed skin. There is usually not much depth to a Stage II ulcer. The wound appears like a scrape or blister with a shallow wound bed.
Similar to a Stage 1, litigation does not usually arise out of Stage 2 ulcers since they are not cavernous wounds. Stage II pressure injuries can be treated and healed if caught early enough.
What is a Stage 3 Pressure Ulcer?
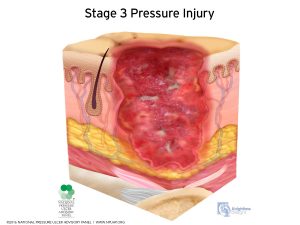
A stage 3 pressure ulcer is a more serious wound with an appreciable depth. At this point, the wound has cratering and extends into the fat which is underneath the skin. A stage 3 pressure injury does not reach tendon, muscle, or bone though. A stage 3 pressure wound poses a serious health risk to the patient and should be treated by an outside wound care team.
What is a Stage 4 Bed Sore?
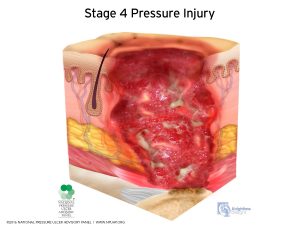
A Stage 4 bed sore is a severe, cavernous wound that poses a clear and imminent danger to the patient. Stage 4 bed sores are very deep, with the pressure injury reaching depths into the muscle and bone. Damage to deeper tissues, tendons, and joints are possible and a stage 4 pressure injury may get infected with osteomyelitis.
The majority of bed sore cases handled by our bed sore attorneys involve stage 4 pressure ulcer claims. Due to the severity of this kind of bed sore, lawsuits commonly arise out of stage 4 pressure injuries. A stage 4 pressure ulcer should not go unpunished and without investigation.
What is an Unstageable Bed Sore?
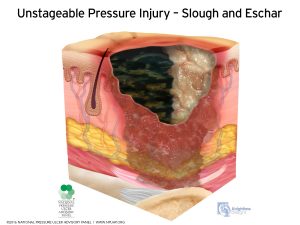
An unstageable bed sore is so severe that the depth of the wound cannot be seen. Since these pressure injuries are staged based on depth, the wound is unstageable because the bottom is covered by liquid or slough. Unstageable wounds are oftentimes Stage 4 wounds that are so deep, the depth of the pressure injury cannot be measured.
Our bed sore lawyers regularly accept representation on cases involving unstageable wounds, as they are oftentimes just as severe as stage 4 pressure injuries.
What is a Deep Tissue Injury?
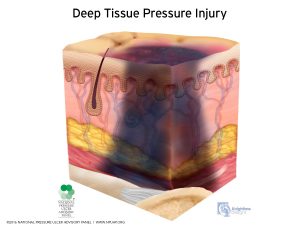
A deep tissue injury is a bed sore that develops from within. This means the insult to the skin occurs inside while the outside skin remains intact. A deep tissue injury (commonly called a DTI) then opens up and reveals a deep wound. A DTI may appear purple or maroon before opening up.
Sometimes a nursing home will classify a pressure ulcer as a DTI in order to avoid liability for a large wound. We see this frequently in charts where a resident arrives to the facility with intact skin, and develops a deep Stage 4 pressure ulcer in the facility. In an attempt to avoid accountability for the wound, nursing home staff chart the wound as a preexisting deep tissue injury.
Why Staging a Bed Sore Matters
If you are unsure which stage wound your family member has developed, speak with our bed sore attorneys today so that we can obtain the relevant medical records and determine the stage of the wound. The stage of the wound determines the treatment options available. Additionally, more severely staged wounds, like Stage 3, Stage 4, and unstageable wounds, trigger mandatory reporting events.
Am I Allowed to Take Pictures of My Parents Bed Sore?
Absolutely. In fact, we recommend you photograph your loved one’s wounds. Documenting your family member’s wound with photographs is crucial. They say a photograph is worth a thousand words. This is true in bedsore neglect claims. Pictures of the wound are necessary to prove 1) that a bedsore existed and 2) to date when the bedsore developed. Bed sore pictures can be used against the nursing home or hospital later in court.
Never rely on the facility to document the bedsore with photographs! Even if you see the wound care team taking pictures of the pressure ulcer, do not assume that those photos will make it into the medical record. Be sure to document the wound yourself by taking your own photographs, which can serve as evidence later on in your nursing home abuse claim.
Bed Sore Statistics in Nursing Homes and Hospitals
According to the Centers for Disease Control, more than 10% of patients residing in nursing homes suffer from pressure sores. Of those patients, 50% of them had a Stage III or Stage IV bed sores, which means that it was a severe pressure ulcer. Pressure ulcers are a ‘never event’ in hospitals and nursing homes. This means pressure sores should never occur inside a facility and there is usually no excuse for bedsore formation.
As many as 11% of all nursing home residents have at least one pressure ulcer. Unfortunately, of these, only 35% received the appropriate care to address their wounds. Pressure ulcers can be deadly when not appropriately treated. In fact, individuals with pressure ulcers are 2 to 6 times more likely to die from them than from other high-mortality issues such as cardiovascular disease and cancer. Some studies show that at certain facilities, the rate of pressure ulcers in residents could reach as high as 91%. 60% of patients who experience a serious pressure ulcer pass away in the 12 months following the injury.
The most common victims of bedsores are patients over the age of 60 who have compromised mobility. When a patient has compromised mobility, it means that they cannot move or reposition themselves in bed. Statistically, bedsores occur far more often in nursing homes versus hospitals or in-home elder care. This is likely due to systemic understaffing in America’s nursing home industry. If there are not enough nurses working on a facility floor, not all the at-risk patients will be turned and repositioned. When patients are neglected and left lying in bed in their own urine and feces, infected bedsores develop. Although statistically most bed sore sufferers reside in nursing homes, hospital-acquired bedsores do occur and are usually due to patient neglect as well.
According to bed sore statistics, the most common cause of skin breakdown is the failure to turn and reposition the patient. Dehydration and malnutrition are the second leading cause of pressure injuries.
Shockingly, patients are more likely to develop pressure sores in today’s nursing homes and hospitals than at any other time. With budget cuts and realignments in the medical sector, facility nurses are understaffed. Nurses are also under-trained and doing jobs for which they are not qualified, resulting in inadequate care of patients, which is unacceptable. Studies such as those documented in the National Library of Medicine National Institution of Health stated that patients admitted to hospitals from a nursing home were more than five times more likely to have pressure sores.
The average cost of treating a bedsore—about $37,800—disincentivizes adequate treatment. This is why filing a lawsuit to secure damages and hold the facility accountable is important; it can serve to force them to adapt their methods, saving other residents in the future.
Who is at Risk for Bed Sores?
As mentioned above, nursing home residents are more likely to develop bedsores than hospital patients. This is because nursing home staff numbers are lower, and the general care in these facilities is lower than that of an acute care hospital.
Potential risk boosters of bedsores in nursing homes and hospitals include:
- Aging – elderly people have thinner skin, which vastly increases their risk of getting ulcers.
- Lack of pain receptors – some elderly people have nerve disorders that prevent them from feeling the pain and discomfort that lets a person know they need to change their position in bed.
- Incontinence – the moisture associated with incontinence can boost the chances of developing pressure injuries. Urine and feces also add to the risk of infecting the pressure ulcer wound.
- Malnutrition – deficiencies in certain nutrients can skyrocket your chances of developing a bedsore and makes developed bedsores harder to treat.
- Diabetes or vascular disease – Diabetes, Peripheral Vascular Disease (PVD) and Peripheral Arterial Disease (PAD) accelerate wound development. Further, these diseases compromise blood flow and make existing bed sores harder to treat. However, vascular blood flow insufficiencies are not excuses for pressure ulcer development.
- Smoking – nicotine acts in a similar way to circulatory diseases, restricting blood flow and not allowing proper circulation to the affected area.
How Does Nutrition Impact Bed Sores?
The medical community is in agreement that improper nutrition can contribute to bed sore development.
Malnutrition appears to be a common contributor to bedsore occurrence in nursing homes, but other less severe nutritional deficiencies can also make bedsores more common. This is why it is crucial that the nursing home staff carefully monitors the patient’s nutrition levels in order to prevent skin breakdown. Repositioning a patient is not enough to prevent skin breakdown. The facility must ensure that the patient is getting appropriate nutrition and hydration as well.
A balanced diet can not only reduce the likelihood of bedsores developing, but also significantly improve healing times of existing bedsores.
The nutritional deficiencies that increase bedsore risk are:
- Protein
- Zinc
- Vitamin C
These increase your risk because they are crucial for the strength of your skin and your body’s ability to heal.
Try to make sure your family member is getting more of the following:
- Meat, eggs, and dairy – for protein and zinc
- Fruits and vegetables – for vitamin C
If the patient is unable to eat solid foods, speak with the facility’s nutritionist about setting up feeding alternatives. A recent study shows the positive effect that nursing home patients with bedsores experienced after undergoing a nutrition intervention. When the nutrition experts took control of the patients’ nutrition, bedsore healing rates were significantly higher. This was likely because they were getting enough of these nutrients compared to their previous nursing home diet.
Pressure Ulcer Prevention in Nursing Homes

Preventing pressure sores in nursing homes and hospitals is a relatively straightforward task. If a nurse is on top of providing the required care to the patient, a bedsore will not form. Unfortunately, nursing homes often fail to reposition immobile individuals every two hours, fail to properly place cream on existing small pressure sores, and fail to give proper nutrition intervention to those at risk. This allows bedsores to form.
Here is a quick checklist that can be used to prevent bedsores in nursing homes, hospitals, and assisted living facilities:
- Reposition the patient at least every two hours in bed and every 15 minutes in a wheelchair
- Place special creams on bedsore to help the wound heal and stay clean
- Use a donut cushion when the patient is sitting in a chair or wheelchair
- Utilize a special air loss mattress to offload pressure of the affected area
- Use a wound vac on existing pressure ulcers
- If the wound is severe enough, plastic surgery can be performed to close off the wound and prevent further infection and deterioration
Pressure injury prevention is the responsibility of the facility. As a layperson, knowledge is power. The best thing to do is to equip yourself with the knowledge about bedsore prevention and communicate with the facility so that they provide the appropriate standard of care to your family member.
You should ask questions and raise concerns if you feel your family member is being neglected. Visit at different times and never announce your presence to staff. Monitor whether your family member is in the same position throughout the day. Check to make sure their clothes and adult briefs are clean. Always inspect their skin for areas of breakdown, and if you notice a bed sore, bring that wound to the attention of nursing. Remember though: appropriate care is their responsibility, not yours.
What To Do When Caregivers Fail: Bed Sore Lawsuit

Pressure sore lawsuits are becoming increasingly common in the US, primarily because healthcare experts agree there is no reason for many bed sores to occur. Our elder abuse attorneys file more bed sore lawsuits than any other type of injury claim.
There is simply no justification for these kinds of skin insults to develop in a hospital or healthcare facility.
If a nursing home has a bedsore problem, there may be a larger, facility-wide, systemic patient neglect problem. By opening a bed sore claim, you are exposing this potentially pervasive problem in the facility.
If you have a potential bedsore lawsuit, contact an attorney focusing on elder abuse cases. Our bedsore lawyers have handled thousands of cases involving this specific kind of injury.

Most bedsores develop due to negligence on the part of hospital or nursing home nurses. Tragically, this cycle continues because only 1 in 14 incidents of elder abuse in the U.S. actually gets reported. This allows the negligent facilities to continue to neglect their patients, thereby creating more bed sores and resulting injuries.
At Senior Justice Law Firm, our lawyers have years of experience litigating bedsore negligence lawsuits. Our bed sore attorneys have recovered millions of dollars for our clients in neglect cases. We understand how enraging a preventable pressure ulcer can be, especially considering the lethal health impact it can have on an elderly patient. We understand that these cases are about much more than just money; they are about justice.
Now Is the Time to Take Action
If your loved one developed bed sores, take action. Don’t allow other patients in the facility to suffer the seemingly endless cycle of elder abuse. Be a voice for the voiceless and stand up to patient neglect.
If your family member suffered any of the following injuries, contact our firm immediately.
- Pressure Sores
- Falls Resulting in Broken Bones
- Brain Bleeds
- Unexplained Broken Bones
- Significant Weight Loss
- Sepsis
- Amputation
- Choking Death
- Medication Mistakes
- Patient Wandering out of the Facility
- Sexual Assault & Abuse
- Physical Attacks
- Wheelchair Transfer Injuries
- Pneumonia
- Aspiration Pneumonia
- Infections
- Urinary Tract Infections
- Wrongful Death
Speak With a Compassionate Bed Sore Attorney Now, For Free
Contact us now for your free case consultation at 1-888-375-9998 or by live chatting with our law firm today.
Bed Sores Questions and Answers
Page updated 11-10-2021.

