Connecting Nursing Home Understaffing to Injury & Wrongful Death
Nursing home understaffing is the root cause of most nursing home injuries.
When a facility or its corporate owners intentionally short staff a nursing home, this leads to preventable errors, nursing mistakes, negligence, and resident neglect.
Our nursing home attorneys handle nursing home negligence lawsuits nationwide. Unfortunately, when we accept a case and investigate the facility’s staffing levels, we oftentimes find that the facility was understaffed. The lack of nurses and aides causes preventable injuries, such as bed sores, resident falls, untreated infection, and wrongful death.
Free Case Consultation – Speak with our Experience Nursing Home Attorneys Now:
888-375-9998
How to Recognize Understaffing in Nursing Homes
 Understaffing in nursing homes is not easily detected. Further, state agencies do not always enforce staffing standards, so facilities get away with understaffing. Despite there being numerous federal and state measures in place to regulate the staffing of nursing homes, it can be difficult for surveyors to enforce staffing standards.
Understaffing in nursing homes is not easily detected. Further, state agencies do not always enforce staffing standards, so facilities get away with understaffing. Despite there being numerous federal and state measures in place to regulate the staffing of nursing homes, it can be difficult for surveyors to enforce staffing standards.
Recognizing nursing home understaffing can be challenging, but there are some signs to watch for.
- There may be less staff scheduled to work on weekends than during the week.
- There may be a “skeleton crew” of staff at night. Understaffing during the nightshift is a common issue. While many residents may be asleep in their beds, there could still be instances of injuries or other emergencies that nursing staff need to tend to. Nursing home corporations understaff the night shift since it is more expensive to staff night nurses, and visitors are not there to observe the substandard conditions.
- Call bells and lights may take long periods of time to be answered.
- Family members may frequently call the facility for updates on their loved ones and do not receive responses back.
- Injuries and infections may not be addressed as quickly as they should be. Sometimes, injuries may not be reported at all.
- Staff in the facility may seem extremely stressed and tired. This could be due to them working overtime and caring for more patients than they can handle. Exhausted caretakers are more likely to make medication errors, take their frustration out on residents, and take more time to respond to emergencies.
- Residents may be left alone in their rooms for long periods of time without anyone checking in on them.
If you want to witness the true staff level of a nursing home, try to visit during off hours. Do not announce your intention to visit; just show up to the facility. Visit during the night shift or on weekends to see if the staff levels match those during the weekday day shift.
How Big of an Issue is Understaffing Nursing Homes?
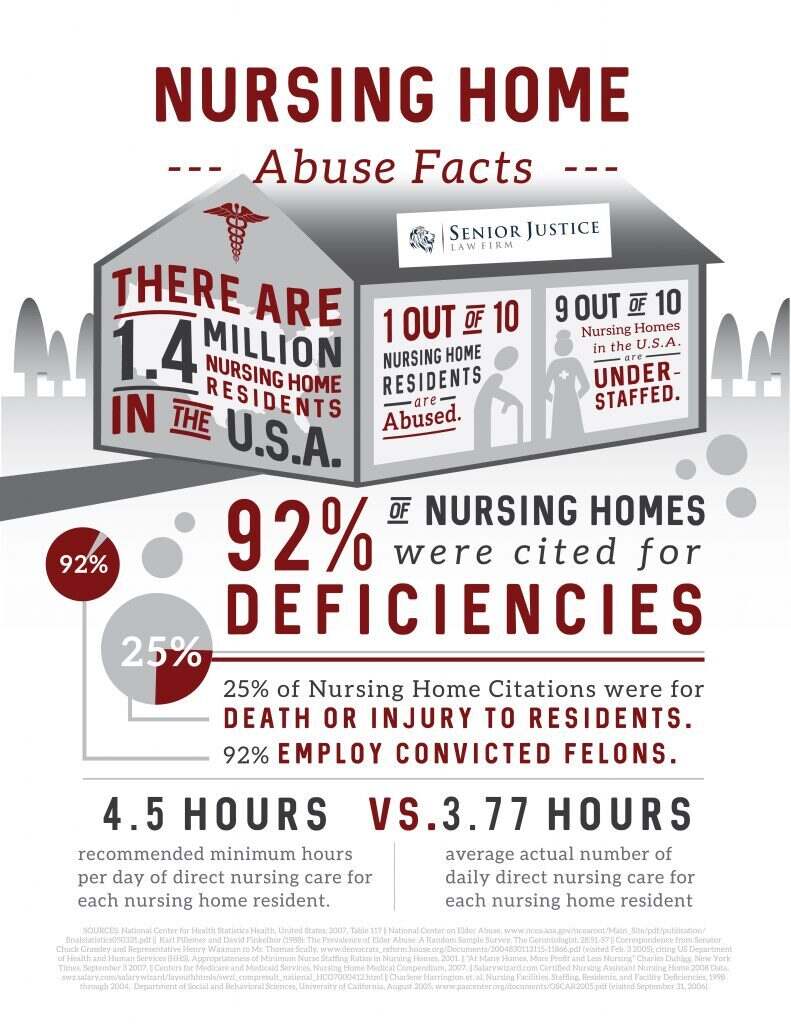 According to a July 2018 article published in U.S. News & World Report, most of America’s nursing homes had inadequate staffing levels at the time. After the Covid-19 pandemic began in 2020, the U.S. witnessed a nationwide nursing shortage that affected hospitals, nursing homes, home health care agencies, and all other medical facilities across the U.S. reported that research has shown as many as 95% of nursing homes in America are now understaffed. It is expected that these staff numbers will not return to pre-COVID levels.
According to a July 2018 article published in U.S. News & World Report, most of America’s nursing homes had inadequate staffing levels at the time. After the Covid-19 pandemic began in 2020, the U.S. witnessed a nationwide nursing shortage that affected hospitals, nursing homes, home health care agencies, and all other medical facilities across the U.S. reported that research has shown as many as 95% of nursing homes in America are now understaffed. It is expected that these staff numbers will not return to pre-COVID levels.
A December 2022 USA Today investigation revealed that thousands of American nursing homes flout federal staffing requirements, and they get away with it. Only 4% of facilities were actually cited for understaffing, despite the fact that most nursing homes intentionally understaff to maximize profits. The investigation echoes what we already know:
“Having enough nurses and aides is the strongest predictor of whether nursing home residents will thrive, researchers have found. When facilities are short-staffed, essential medical tasks are ignored. Doctor’s appointments are missed, call buttons go unanswered, diapers are not changed, showers are not given and wounds are not cleaned. Dementia can set in faster. People get sicker, and die, alone.”
The American Health Care Association investigated and found nearly 90% of nursing home providers report being understaffed, and about 50% are severely understaffed.
There are many different reasons that a nursing home may be understaffed.
For example, hiring less nursing staff means that the cost of labor for management goes down. Less staff means more profit for nursing home owners. This profits before people approach puts the nursing home’s bottom line ahead of resident safety.
There could also be an issue of the nursing home having a high turnover rate. A high turnover rate means that staff are being hired quickly but are also leaving the job quickly. This makes it difficult for the facility to retain adequately trained nurses and CNAs (certified nursing assistants).
Higher staffing levels and lower staffing turnover in a nursing home correlate with higher quality of care for residents. Conversely, lower staffing levels and higher staffing turnover may mean a lower quality of care.
Understaffing is the Nursing Home’s Problem, not the Nursing Home’s Excuse
Skilled nursing facilities intake millions of Medicare taxpayer dollars to care for our elderly and infirm. The nursing home literally tells Medicare or Medicaid how much services were rendered to each resident and receives reimbursement. Overwhelmingly, America’s nursing homes are run by for-profit companies who voluntarily entered the industry, to make money. No one is forcing these corporations to run large chains of nursing homes.
When our attorneys handle a nursing home negligence lawsuit, and we are faced with a defense that the facility could not hire enough staff, it falls on deaf ears.
Adequately staffing the facility is the legal responsibility of the nursing home. If a facility cannot retain or attract enough staff, they should increase their pay or hire agency (temporary) nurses. If this does not work, the nursing home should stop accepting new residents.
When a nursing home fails to adequately staff its facility, this is the defendant facility’s problem. Failing to staff is far from an excuse for negligence; instead, it is the likely cause of the negligence.
Why are Understaffed Nursing Facilities Problematic?
 Nursing homes with inadequate numbers of nursing staff have a much higher chance of neglect-related injury and wrongful death. Residents at understaffed facilities are more susceptible to falls, bedsores, malnutrition, and other injuries.
Nursing homes with inadequate numbers of nursing staff have a much higher chance of neglect-related injury and wrongful death. Residents at understaffed facilities are more susceptible to falls, bedsores, malnutrition, and other injuries.
Chronic understaffing can lead to:
- A greater risk of falls and fall injuries due to the lack of supervision of patients. For example, a resident who needs to urinate may feel shame wetting the bed and press the call bell for help ambulating to the restroom. After waiting for help to come to no avail, the resident decides to try to get to the restroom by themselves. Due to the lack of supervision and lack of assistance, the resident could fall on the way to the bathroom and suffer an injury.
- An increased risk of immobile patients developing bedsores, also known as pressure ulcers or decubitus ulcers. Patients who have trouble moving by themselves need to be turned in bed every two hours to prevent skin breakdown. Understaffing can lead to the development of bedsores because there are not enough staff around to turn patients.
- An increased risk of infections due to not cleaning catheters, diapers, bed sheets, etc. A resident who is constantly left sitting in their wet diapers would be more susceptible to infections like UTIs (urinary tract infections) or infections of pressure ulcers.
- Exhausted staff that take out their frustration on patients. This could result in verbal abuse, emotional abuse, physical abuse, or even sexual abuse.
- Malnutrition and/or dehydration for residents that have difficulty feeding themselves. Some residents in nursing homes may require help eating or lifting a cup to their lips to drink. When a facility is understaffed, these residents may not receive the help they need to be well-fed and hydrated.
- Difficulty handing out medications on a routine schedule. Not receiving medications on time could aggravate a resident’s medical condition(s).
- Residents suffering from poor hygiene. Residents in understaffed nursing facilities may not be bathed regularly and may not receive nail care.
Nursing Homes are Underreporting Resident Injuries
A recent national study was completed by a group of researchers from the University of Chicago on the accuracy of nursing home-reported data given to The Centers for Medicare and Medicaid Services (CMS). The assessment focused mainly on the underreporting of pressure ulcers to CMS. The results of the study showed that almost half of residents’ pressure ulcers went unreported to CMS. Furthermore, findings showed that residents’ falls were underreported as well. Only 57.5% of major fall injuries resulting in a hospitalization (such as a broken bone, fracture, or brain bleed) were reported to CMS. As for hospital visits- only 70% of short-term hospitalizations and 60% of long-term hospitalizations were reported by facilities.
Risk Factors for Nursing Home Bedsores
Understaffing in nursing homes can lead to residents developing bedsores, also known as pressure ulcers or decubitus ulcers. Bedsores are preventable and while relatively common nowadays, not normal. A resident living in an understaffed facility may not receive the proper care they need to prevent bedsores from developing. Some risk factors for developing pressure ulcers are:
- Immobility: Residents with limited mobility are more susceptible to developing bedsores due to not being able to reposition themselves in bed or a chair. CNAs or nurses need to turn residents every two hours to offload the pressure on the patients’ bottom, legs, and heels. Someone who is immobile will not be able to relieve the pressure off certain parts of their body without adequate help from a staff member. If a facility is understaffed, residents at risk for pressure wounds will not receive the help they need.
- Incontinence: Residents who do not have control over their urinary or bowel function may be at risk for skin breakdown. If incontinent residents are not kept clean after going to the bathroom, their skin on their buttocks and genitals can begin to breakdown and form a wound.
- Lack of sensory perception: People who have lost feeling or have become paralyzed due to a brain or spinal cord injury may not be aware of the development of a bedsore on their body. Without help to offload the pressure in the area where the bedsore has developed, the wound will continue to worsen and could become infected if not kept clean.
- Poor nutrition and dehydration: Without enough fluids, calories, and protein, skin breaks down easier and quicker. There is a risk of suffering from skin breakdown in an understaffed facility where residents may not be receiving enough to eat or drink. Wound care doctors commonly put their patients on a high-protein diet to help heal a wound. With a protein-deficit, your body does not have enough of the necessary building-blocks to protect you from skin breakdown.
CMS Calls on States to Give Incentives to Nursing Homes to Provide Better Care
An informational bulletin was put out on August 22, 2022, by the Centers for Medicare and Medicaid Services (CMS). The purpose of the bulletin is to outline CMS’ commitment to working with states to develop payment methodologies that incentivize improving the quality of health care services provided to residents in long-term care facilities. The bulletin builds on a set of reforms announced by the White House in February of 2022 (Biden-Harris Administration’s Nursing Home Reform Action Plan) to improve the quality of care that nursing home residents receive.
Some states, such as California and Illinois, have already begun to implement Medicaid payment initiatives. Illinois’ new nursing facility payment initiative focuses on staffing incentives and supports facilities in increasing and maintaining the wages of CNAs (certified nursing assistants) through the “CNA Tenure and Promotion Payments.” This initiative has increased staff retention levels which could lead to better quality of care for residents. California’s payment initiative provides increased payments to nursing homes that meet or surpass the statewide average of quality care (which is measured by a set of quality indicators defined by CMS).
The Effect of the Covid-19 Pandemic on Nursing Home Staffing
Human Rights Watch, a nonprofit organization that reports on the rights of people worldwide, released an article in March of 2021 about the concerns of nationwide neglect in American nursing homes. When Human Rights Watch interviewed nursing home staff and administrators, they were told that understaffing affected the nursing staff’s ability to provide adequate care to residents. Staff also reported to journalists that prior to the Covid-19 pandemic, they expected residents’ families to assist with their daily care. When nursing homes were shut-off from visitors due to the pandemic, families were not there to help take care of their loved ones, and staff were too overwhelmed to care for an abundance of residents. In essence, the Covid-19 pandemic exacerbated already existing shortfalls in nursing home regulation.
What You Should Do If You Suspect Nursing Home Understaffing
If Your Loved One Has Not Yet Been Injured
If you think your family member’s nursing home is short-staffed, but they have not been physically harmed by the lack of attention, schedule a meeting with facility management to discuss your concerns. Do not let them talk around the issue by claiming “we staff above state minimums.” These are state minimums, and federally, the regulations require that nursing homes staff to the acuity of the resident. This means if a resident is high acuity (high needs), they require more staff attention. If they are not getting the attention their acuity requires, the facility is likely understaffed. Consider relocating your loved one to a higher staffed facility. Use Medicare’s nursing home compare tool to analyze local nursing home staffing data in your zip code.
If Your Loved One Suffered Injury, or Wrongful Death
If your loved one unfortunately suffered an injury or death inside the facility, this may have been caused by a lack of nursing home staff. We have seen all kinds of horrific incidents occur in skilled nursing facilities – choking deaths, resident fights, pressure ulcers, falls, medication errors, elopement from the facility – all attributable to a lack of staff to supervise and assist the at-risk residents.
You should report the incident to your local Ombudsman and/or department of health. If you need assistance with this, our legal team can help.
Additionally, you should speak with the lawyers at Senior Justice Law Firm. We narrowly focus our practice on claims against nursing homes and this specialized niche allows us to really make an impact on the cases we pursue. Call us today to learn more about how we can help, what legal rights you have, and why our firm is different: 888-375-9998
Did Understaffing Cause Your Loved One’s Injury or Wrongful Death?

Contact the experienced nursing home abuse attorneys at Senior Justice Law Firm. Our skilled lawyers narrowly focus on elder abuse claims, and we routinely analyze the staffing levels at the defendant nursing facility. Our attorneys regularly retain nursing home staffing experts who opine on technical subjects, like the appropriate staff level at the nursing home at the time of the incident.
Analyzing the staffing levels at a skilled nursing facility is a daunting task. Let our experienced attorneys guide you along your journey to justice.
Submit your case facts below, live chat with our office now, or call us for a completely free case consultation: 888-375-9998


