Understanding the Connection Between Osteomyelitis and Infected Bed Sores
Osteomyelitis from Infected Pressure Wounds is Strongly Correlated with Nursing Negligence and Patient Neglect
Getting older is not easy on the body. However, when our loved ones reside in nursing homes, assisted living facilities, or in a hospital, certain kinds of injuries are not supposed to occur. Neglect-related injuries, such as infected bedsores or pressure ulcers, are a “never event” in healthcare. This means they should never occur.
If you recently learned that a loved one in a nursing home has been afflicted with osteomyelitis, you might not understand what that means or what you should do about it. However, many cases of osteomyelitis in nursing homes can be traced to improper care and, in particular, the presence of infected bedsores. Osteomyelitis from infected pressure ulcers are a strong indicator of nursing home abuse.
Free Osteomyelitis Pressure Ulcer Lawsuit Case Consultation
Free Osteomyelitis Case Consultation: (888) 375-9998
Before you read any further, pressure injuries infected with osteomyelitis are almost never acceptable. If a family member developed osteomyelitis in a pressure wound while living in a healthcare facility, call Senior Justice Law Firm today. Our narrowly focused bed sore attorneys specialize in these kinds of cases and we can help your family get justice for this preventable infection. Receive a completely free case consultation by calling us at (888) 375-9998 or live chat with our office now using the box on your screen.
What Is Osteomyelitis, and How is it Related to Infected Pressure Ulcers?
Here’s what you need to know about the connection between osteomyelitis and pressure sores, how it happens, and what you can do about its causes.
If your loved one has been diagnosed with osteomyelitis, you may not even realize it until a physician breaks the bad news. In fact, you may have only been told that they are experiencing inflammation surrounding their bones or that they have a bone infection.
How does bone get infected, especially in a nursing home?
Osteomyelitis is caused when bacteria is able to wedge its way into the bone and settle. Once inside the bone structure, this bacteria multiplies, causing pain and inflammation. This condition is a type of infection, which means that it can become more serious or even fatal if left untreated. This is especially problematic among nursing home residents, whose immune systems tend to be weaker as a result of age, medications, or a combination of the two.
How Does Osteomyelitis Colonize Bone in Elderly Patients?
Pressure ulcers act like a gateway for the bacteria to enter an elderly person’s body.
There are many ways that osteomyelitis can begin, but the bloodstream is the primary path that bacteria will take to spread. Most often, the bacteria responsible are staphylococcus, which even healthy people have in abundance on their skin and usually in their nose.
Normally, the skin would act like a barrier to keep this harmful bacteria from entering the blood stream. However, when an open wound allows these existing staph bacteria in, bacteria can travel to the bone, colonize, set in the bone, and cause bone infection called Osteomyelitis.
Osteomyelitis Infection May Not Be Geographically Near the Pressure Sore
What complicates matters is that the bloodstream spans the entire body, and staphylococcus bacteria are free to roam anywhere they like once they have entered the blood. This means that osteomyelitis could occur anywhere, even far away from where the original pressure wound happened. It can be confusing to see someone get a bone infection in their foot when they have an open wound on their backside.
However, the most frequent occurrence is that the staph bacteria does not travel far. Instead, they migrate directly inward from the pressure injury and affect the bone nearby. Your loved one is susceptible to osteomyelitis if they have experienced an open injury, especially one that remains open or is not regularly disinfected and treated.
Osteomyelitis in Nursing Home Patients is Strongly Connected to Pressure Ulcer Rates
Sadly, the incidence of osteomyelitis in nursing homes is far greater than the general population, and for one important reason: neglect. While it is true that elderly individuals tend to have a weaker immune system overall, the driving factor behind the higher number of osteomyelitis cases in care facilities is due to their correspondence with bedsores.
A bed sore is a type of injury that arises when pressure is placed on an area for an extended period of time. As you may imagine, this is a consistent challenge in nursing homes, when compromised individuals spend most of their day in bed. Nursing facilities are legally required to check on residents every few hours to help them shift their body weight so that pressure ulcers do not arise. This is called turning and repositioning and must be done in immobile patients that are in bed or in a wheelchair.
The standard of care is that at-risk residents get turned and repositioned in bed every two hours. Sadly, this does not happen at many nursing homes and the result is skin breakdown in the form of pressure injuries.
Why Do Nursing Homes Ignore Turning & Repositioning At-Risk Patients?
Most nursing homes are understaffed, and this constant checking in is one of the easiest tasks to neglect. Understaffed nursing homes statistically cause preventable injury. Thus, pressure injuries form, resulting in an open wound. These bedsores can reach all the way to the bone if left untreated—providing an open wound into which staphylococcus are easily able to enter, and with a clear path directly to bone tissue.
For this reason, osteomyelitis is closely associated with bedsores, and nursing homes that struggle to provide adequate care for their residents are more likely to see an uptick in both pressure ulcers and bone infections as a result.
The Risks and Causes of Bone Infection Via Pressure Ulcer Injuries
Pressure ulcer injuries are caused by a person’s bodyweight bearing down on skin tissue for too long. This most often occurs in areas of thin skin, with the sacral region (near the buttocks, at the base of the spine) and the heels as the most vulnerable. It is critical to remember that bed sores are generally preventable. There is no medical condition that causes them as one of its symptoms. Pressure ulcers only happen when the nursing home is not providing an adequate level of care to its residents. In other words, pressure injuries are directly related to abuse and neglect in a facility.
Given this, it is easier to understand how osteomyelitis is associated with abuse and neglect as well. Many bone infections would be completely averted if their originating pressure ulcers never happened. It is no coincidence that the most common type of osteomyelitis in nursing homes occurs in the pelvis—where the most common type of bedsore also appears near the coccyx or sacrum area. In addition to the risk of osteomyelitis, the bedsores themselves are also of great concern for a resident’s health.
Sacral Pressure Ulcers Near the Coccyx Pose a Particular Risk for Osteomyelitis
 Because pressure ulcers continue to grow until their cause is treated and the resident receives better care, they can be difficult to manage once they appear. Naturally, they are a prime area for infection to begin, especially sacral pressure ulcers.
Because pressure ulcers continue to grow until their cause is treated and the resident receives better care, they can be difficult to manage once they appear. Naturally, they are a prime area for infection to begin, especially sacral pressure ulcers.
Bed sores on a patient’s buttocks pose particular risk of Osteomyelitis because they are open, and anatomically near the patient’s genitalia. This means, if the patient is neglected, they will frequently sit in their own waste. Feces and urine can increase the odds of bone infection via the pressure ulcer.
Unfortunately, a pressure ulcer near the coccyx or sacrum will likely be exposed to fecal contamination if the patient is incontinent and neglected by nursing staff.
Recognizing Infection and Osteomyelitis in Pressure Injuries
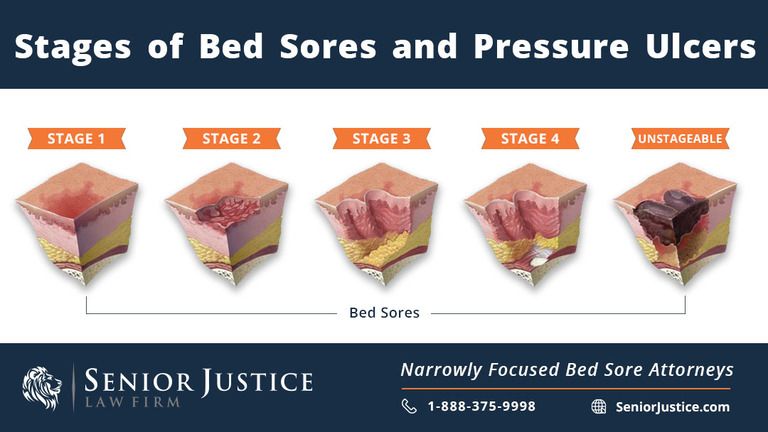
Infected pressure ulcers can also be the source of severe bleeding and unmanageable pain. Remember—stage 4 bedsores can be wide and deep enough to extend to the bone. The resulting pain and damage from the injury will naturally be significant. The tissue around the bedsore may begin to turn necrotic and die, resulting in a slow spreading of the injury. In addition to infiltrating the bone, any infection in the sores can also spread to the joints in a condition called septic arthritis.
Osteomyelitis presents with erythema (reddening of the skin), exudate (liquid or pus discharging from the wound), and purulence (discharge or liquid in the wound).
Doctors diagnose osteomyelitis from a pressure ulcer by analyzing lab results, specifically looking at ESR and CRP markers, and by conducting an MRI or bone biopsy.
What You Can Do if an Infected Pressure Ulcer Leads to Osteomyelitis
If someone you love has been diagnosed with osteomyelitis, you might not know what to do next—especially if you are already aware that your family member has bedsores. Whether or not they do, the nursing home may try to explain that bone infections happen from time to time and are nothing of concern. It is important that you delve deeper into the cause.
Osteomyelitis is closely related to poor standards of care in nursing homes. While it is certainly true that sometimes bone infections in the elderly can occur from unexpected or even unknown injuries (like a cavity in a tooth), more often, in nursing home residents, osteomyelitis can be traced to negligent behavior from a facility. You may report this abuse to local authorities or your regional ombudsman as a good first step.
Benefits of an Osteomyelitis Nursing Home Lawsuit
In addition to reporting the neglect, it is also worth considering legal action. A lawsuit against the nursing home for allowing your loved one to develop osteomyelitis will afford your family an avenue for justice.
You may be able to recover monetary damages for not only the pain and suffering that your loved one endured but also medical bills and other expenses that were paid to treat the pressure ulcer and corresponding osteomyelitis. As an additional benefit, your lawsuit can make a substantial difference in the lives of other residents of the nursing home.
Why Nursing Home Osteomyelitis Lawsuits Change Care for the Better
The majority of nursing facilities are for-profit locations that run on a profits-first mentality. This has driven many nursing homes to prioritize and streamline their administration to increase their profits at the expense of the residents who live there. Perhaps they try to get away with hiring fewer staff. Maybe the staff they hire are uncaring or inattentive because they pay them cheap wages. Maybe the nursing home scrimped on medical equipment which could have prevented the pressure wound.
Whatever the corporate decision, the decision is usually made in order to make more money. By filing an osteomyelitis pressure ulcer lawsuit against the negligent nursing home corporation, you subject the company to financial difficulties. You have the ability to make nursing home neglect too expensive to ignore. When they pay your family a large settlement, it becomes cheaper for them in the future to provide better care and not allow residents to develop pressure ulcer infections.
In an effort to avoid such costs in the future, nursing homes may amend their practices. Thus, by filing a lawsuit, you can improve the care and conditions of other residents and force the facility to adapt as a result of what your loved one experienced.
Free Osteomyelitis Nursing Home Case Consultation
At Senior Justice Law Firm, we understand that this is an emotional time, and that a lawsuit might be the last thing on your mind.
That’s why we try to make things as simple as possible. Share your story during a free consultation with the confidence that we work on contingency. We will never collect money from you unless we make a recovery in your case, from which we will simply take a percentage. This ensures that anyone, no matter their financial situation, has access to the justice that they deserve. Reach out to learn more about how Senior Justice Law Firm focuses solely on nursing home abuse and neglect cases and how we can help you and your family.
Submit your case facts below, or call us now at (888) 375-9998.


