Fatal falls and fall-related injuries are increasing in senior citizens across the United States, according to a recent Centers for Disease Control and Prevention report. The startling statistics serve as a reminder: when older adults fall, the results can be deadly.
Falling is a Frequent Cause of Death in Seniors
Deaths from unintentional injuries are the seventh leading cause of death among older adults, and falls account for the largest percentage of those deaths. – CDC Report
25% of older adults report suffering a serious fall each year and approximately 3 million ER visits annually are due to senior citizen falls.
Just last year, approximately 30,000 US deaths were attributable to adults aged 65 or more falling. This does not include the tens of thousands of falls that resulted in broken hips, fractured pelvis, broken femurs and subdural hematoma brain bleeds. All of these fall-related injuries cause a rapid decline in seniors and can indirectly accelerate their mortality.
85% of fatal falling victims had a prior history of falls. This means, most of the time, fatal falls can be prevented before they occur.
Fall Prevention
To prevent falls in older adults, the root cause of the falling should be determined.
If the fall victim falls in a nursing home, the staff must adjust the care plan to determine how to stop future falls.
If the fall victim falls in an assisted living or memory care unit, facility management must analyze whether the resident is an appropriate candidate for the ALF due to their falls.
If the person resides independently, he or she should have a conversation with their doctor about how to prevent future falls.
Techniques to Stop Senior Falls
- Home safety interventions, such as removing clutter from walkways and making sure hallways are wide and unobstructed.
- Remove rugs from bathrooms, kitchens and walkways.
- Proper footwear.
- Assistive devices, such as a cane, walker or wheelchair.
- Getting the older adult’s vision tested to determine if they need corrective lenses.
- Cataract surgery, if indicated, greatly reduces falls in patients aged 65+.
- Podiatrist evaluation to examine whether a foot or ankle disorder is causing falls.
- Holistic treatments, such as Tai Chi or Vitamin D.
- Physical therapy to strengthen muscles used in walking.
- Use of a call button or LifeAlert pendant.
- Pacemakers in seniors with cartoid sinus hypersensitivity.
- Changing the patient’s medication administration to reduce confusion.
- Installing handrails on walls and carpet in high-fall risk areas.
- Floor mats to avoid fractures if a fall occurs.
- Bed alarms and chair alarms to beep when a confused senior gets out of their bed/chair without assistance.
Senior Falls are on the Rise in Almost Every Demographic
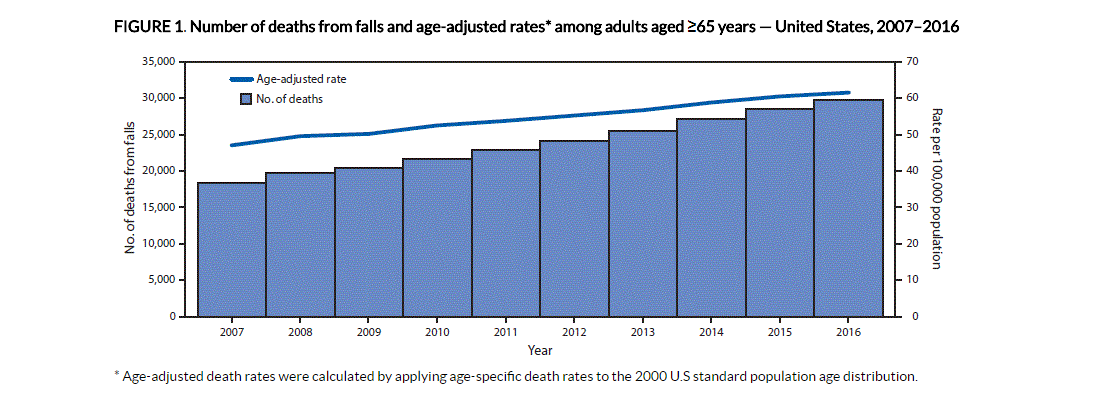
Americans are living longer. This means that older adults are up and walking with more fall-risk factors, such as unsteady gait, shuffling feet, confusion and circulatory problems. As a result, the rates of senior falls have increased across every demographic of society.
Senior Fall Statistics Provided by the CDC
| TABLE. Number and age-adjusted rates* for deaths from falls and annual percentage changes† among persons aged ≥65 years, by selected characteristics — United States, 2007–2016 | ||||||
| Characteristic | 2007 | 2016 | 2007–2016 | |||
| No. of deaths | Deaths per 100,000 (95% CI) | No. of deaths | Deaths per 100,000 (95% CI) | APC (95% CI) | ||
| Total | 18,334 | 47.0 (46.4–47.7) | 29,668 | 61.6 (60.9–62.3) | 3.0 (2.8–3.2) | |
| Sex | ||||||
| Men | 8,408 | 57.9 (56.7–59.2) | 13,721 | 72.3 (71.1–73.5) | 2.4 (2.1–2.7) | |
| Women | 9,926 | 40.2 (39.4–41.0) | 15,947 | 54.0 (53.1–54.8) | 3.8 (3.2–4.4) | |
| Age group (yrs) | ||||||
| 65–74 | 2,594 | 13.2 (12.7–13.7) | 4,479 | 15.6 (15.2–16.1) | 1.8 (1.3–2.3) | |
| 75–85 | 6,552 | 50.1 (48.9–51.3) | 8,735 | 61.4 (60.1–62.7) | 2.3 (1.8–2.7) | |
| ≥85 | 9,188 | 182.3 (178.6–186.0) | 16,454 | 257.9 (253.9–261.8) | 3.9 (3.7–4.0) | |
| Race/Ethnicity§ | ||||||
| White, non-Hispanic | 16,609 | 50.7 (49.9–51.4) | 26,370 | 68.7 (67.8–69.5) | 3.4 (3.2–3.6) | |
| Black, non-Hispanic | 595 | 19.9 (18.3–21.5) | 1,089 | 27.1 (25.5–28.7) | 3.2 (2.1–4.4) | |
| American Indian/Alaska Native | 74 | 47.3 (36.9–59.8) | 111 | 47.0 (38.1–55.9) | −1.5 (−3.6–0.6) | |
| Asian/Pacific Islander | 343 | 31.1 (27.8–34.4) | 738 | 36.7 (34.0 –- 39.4) | 1.5 (0.7–2.4) | |
| Hispanic | 681 | 32.4 (29.9–34.9) | 1,296 | 35.7 (33.8–37.7) | 1.2 (0.2–2.2) | |
| Urban/Rural status¶ | ||||||
| Large central metro | 5,008 | 47.4 (46.1–48.7) | 7,442 | 57.0 (55.7–58.3) | 2.2 (1.9–2.4) | |
| Large fringe metro | 3,990 | 44.0 (42.7–45.4) | 7,000 | 59.9 (58.5–61.3) | 3.4 (2.6–4.2) | |
| Medium metro | 4,008 | 48.3 (46.8–49.8) | 6,879 | 66.1 (64.5–67.7) | 3.3 (2.9–3.7) | |
| Small metro | 1,918 | 49.3 (47.1–51.5) | 3,186 | 66.4 (64.1–68.7) | 3.3 (2.5–4.0) | |
| Micropolitan (non-metro) | 1,976 | 49.6 (47.4–51.8) | 2,970 | 64.2 (61.9–66.6) | 2.8 (2.4–3.3) | |
| Non-core (non-metro) | 1,434 | 44.9 (42.6–47.2) | 2,191 | 60.9 (58.3–63.5) | 3.3 (3.0–3.7) | |
Source: CDC, National Vital Statistics System, Mortality. CDC WONDER. https://wonder.cdc.gov/.
Fall Risk Factors for Older Adults
- Prior fall history
- Confusion, Alzheimer’s or Dementia
- Unsteady gait
- Incontinence of bladder and/or bowel
- Prescription drugs
- Heart conditions (a-fib, bradycardia or tachycardia)

