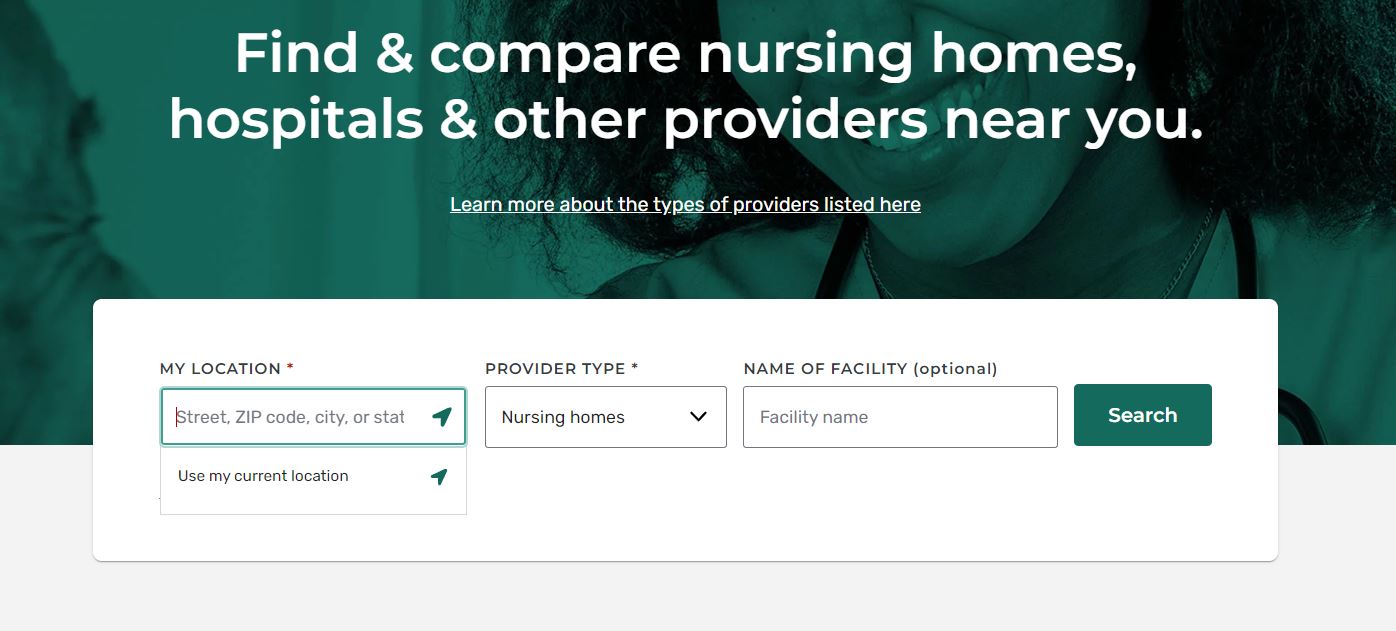
Medicare’s Care Compare tool allows users to compare local nursing homes utilizing Medicare’s 5 star nursing home rating system. However, recent data suggests that Medicare’s 5 star care compare system is deeply flawed and misses many critical reporting areas.
The Data Behind Care Compare: What Is Missing?
In 1998, the Centers for Medicare and Medicaid Services created the Nursing Home Compare database. After consistent issues with nursing home quality, the organization determined that the public did not have enough information to adequately compare different nursing homes when making a selection for their families. Later, in 2003, quality measures were added to multiple sections of the database, such as health inspection results and staffing data.
Studies have indicated that a modest change in the behavior of nursing homes occurred following the introduction of the Care Compare tool, as providers with low scores gradually lost market share and were incentivized to increase their appeal through higher ratings (and thus, better quality). However, the data reflected in the Care Compare tool appears, upon further study, not to adequately reflect certain subsets of information. Further, savvy nursing home owners have learned tricks to game the CMS 5 star system, thereby masking a poorly performing nursing home as a 4 or 5 star facility.
Nursing Homes Game the Medicare 5 Star System
Further research into the ways that the Care Compare database is used has revealed that it is possible for nursing homes to utilize the system to their own advantage—and not just in terms of increasing quality that leads to increased resident application. Many elements of the Care Compare tool are self-reported, and evidence suggests that some facilities inaccurately report data (or obfuscate certain information) to boost their overall rating on the service. Recent changes have made this more difficult in certain areas, such as staffing.
Previously, staffing was self-reported, and so a nursing home could claim to have more staff than they actually employed, or they could boost the number of minutes they claimed that staff spent with each resident. Now, a data collection process based on payroll has been enacted to remove some of this gaming of the system. Still, audits are not regularly conducted on all facilities, and the industry is largely unpoliced on this self-reporting.
Similarly, facilities appear to amend their practices specifically to dominate the Care Compare tool’s 5 star system. For example, if they are aiming for another star in their rating and see that this would be achievable by having their physical therapist work for one more hour, they may do so and nothing else. This encourages facilities to achieve the bare minimum necessary without enacting comprehensive changes to the overall quality of resident care. Thus, a nursing home’s rating may go up with almost no tangible change to the safety of the facility or the robustness of the care that they provide. The facility’s focus becomes on gaining another star; not on resident wellbeing.
The Racial Gap Widens in Nursing Home Care
The other primary issue discovered with the use of the CMS 5 star rating tool is that it has unintentionally exacerbated the disparity of race and Medicaid status in high-quality nursing homes. This comes from a multi-faceted origin. In essence, underserved communities are less likely to find high-quality nursing homes because they are not aware of the tool, which only worsens service in their area, and the cycle continues.
The cause of this phenomenon comes from multiple places. First, nursing homes in low-income areas are more likely to receive a low score. As a result, fewer informed people choose to go to these facilities, which keeps the area low in income, and thus, opportunity. The people who live there—who tend to disproportionately be people of color or individuals lacking online fluency, such as older folks—are less likely to be aware that the Care Compare tool exists, and so they cannot make informed decisions about which nursing homes to trust. They choose the ones closest to them, which usually rank lower than average, and so receive lower quality care than their peers.
In this way, those who already have access to high-quality facilities use the tool to dig in and continue to support (and fill) those more “ideal” locations. Sadly, those with fewer opportunities become entrenched in a cycle of lackluster care.
Studies indicate that the Care Compare tool has worsened this trend by equipping the more fortunate with greater knowledge. Those more fortunate families can travel miles, passing ten skilled nursing facilities, in order to secure a bed at a 5-star nursing home. Conversely, poorer communities that do not leverage the nursing home compare tool simply choose the facility down the road, awarding valuable Medicare dollars to a 1 or 2 star nursing home.
In order to fix this problem, CMS would need to expand outreach and education about the tool to underserved areas.
Missing Data from Medicare’s 5 Star System Leads to Unrepresentative Nursing Home Ratings
The aforementioned problems are not the only challenges faced by the Care Compare data. Over time, it has become increasingly clear that critical metrics are not being measured by the tool.
Missing information includes the quality of end-of-life care, overall family satisfaction, and even patient safety. While a small nod to patient safety does exist in the form of checking for things like fire alarms, there is no information currently in the tool about important safety features (or lack thereof) in a facility, such as:
- Door alarms to prevent elopement
- Bed alarms to prevent resident falls
- Access to call buttons
- Use (or not) of bedrails
- Use (or not) of fall pads
- Reported instances of tripping hazards
- Door locks
- Keycard entry and exit to exterior doors
While this information can sometimes come to light if a violation has been noted in a health inspection, the Care Compare tool does not by itself keep track of it.
Average Rated Nursing Homes are Not Comprehensively Analyzed Under Medicare’s 5 Star Rating System
 Among studies that have examined the efficacy of the Care Compare tool and its benefit (or harm) to the public, the data leads to a consistent conclusion: everything in the middle is the problem. In general, studies show that the Care Compare tool’s ranking of facilities on the extremes (the one-star and five-star locations) is fairly accurate. However, the rest of the facilities in between these bookends are not comprehensively reported on enough to truly understand where they lie.
Among studies that have examined the efficacy of the Care Compare tool and its benefit (or harm) to the public, the data leads to a consistent conclusion: everything in the middle is the problem. In general, studies show that the Care Compare tool’s ranking of facilities on the extremes (the one-star and five-star locations) is fairly accurate. However, the rest of the facilities in between these bookends are not comprehensively reported on enough to truly understand where they lie.
From facilities fudging the numbers to boost their scores to the scores themselves being manipulatable through small and overall inconsequential changes that do not improve quality of life, it seems that CMS could benefit from further refinement to the resource. Ongoing improvement should be the goal, not only to increase the data (and accuracy therein) available, but to mitigate some of the previously unforeseen problems with Care Compare, especially as it relates to the opportunities of underserved and low-income communities.
Ultimately, the 5 star CMS rating system and Medicare.gov’s Care Compare tool are imperfect, but they continue to refine the system to be better than previous versions. While clearly not comprehensive, the nursing home comparing tool allows consumers to have some view into ratings of local skilled nursing facilities.
Nursing Home Abuse Case Consultation
If your loved one was wrongfully injured or died inside a skilled nursing facility, contact Senior Justice Law Firm today for a free case consultation.