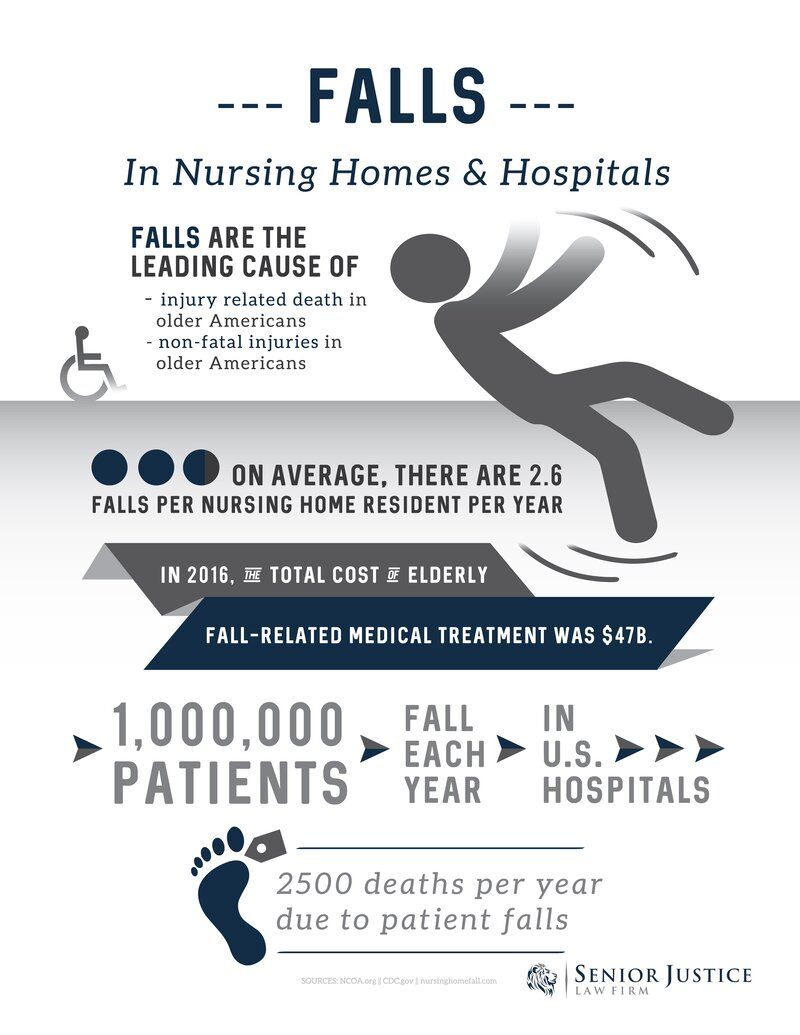
The Connection Between Prescription Drugs and Falls in Nursing Home Residents
A lot of minor injuries can befall an older individual, especially once they migrate to permanent nursing home living. Most families take these mishaps as just a normal part of getting older and give them very little thought. After all, it’s certainly true that older folks tend to be unsteady on their feet compared to their younger years. However, falls in nursing homes are largely preventable, and the culprit behind your loved one’s increased falls might not due to age. There is oftentimes a direct connection between the prescription medication a patient takes and their increase in falls.
In this article, our narrowly focused nursing home abuse and neglect attorneys will analyze how different medications can affect an elderly patient’s risk of falling.
Free Nursing Home Negligence Case Consultation

Our nursing home lawyers have successfully handled thousands of nursing home fall cases like yours.
If your loved one suffered a fall inside a nursing home, hospital, or assisted living facility, contact Senior Justice Law Firm today to learn more about your legal rights. Receive your free consultation by calling (888) 375-9998. You can also live chat with our office or submit your case facts below. All consultations are free and we work on contingency fee, so you pay us nothing out of pocket.
How Does Fall Risk Connect to Medications?
It’s rare that people make the connection between medications and how often their loved ones are falling. However, the reality is that some medications are more likely than others to cause physical symptoms that predispose someone to taking a fall. This could happen because the medication causes dizziness, a drop in blood pressure, or even difficulty seeing.
Behind this connection between falls and medications is the correlation between new nursing home living and a rise in falls. In other words, why do residents who have newly moved into a nursing home seem to be falling so often, especially when they previously had no problems? As it turns out, it’s not just medication but also a potential change in medication that could be playing a role.
Many elderly patients enter a nursing home, and then they begin a new medication regimen. Suddenly, they experience falls more often. If someone you love is taking any of the following prescription medications, be alert for signs that could indicate that your loved one needs assistance with mobility. Preventing falls can save your family member’s life and spare them from pain and permanent disability.
What Prescription Medication Increase Fall Risk in Elderly Patients?
 In order to be on the lookout for increased fall risk in your loved one, you’ll need to pay careful attention to the medications that they take. You should reevaluate their medicine regimen in the nursing home. Many times, small adjustments or additions will be made once they enter a long-term care facility that may not be reflective of the medication they have taken in the past. These small changes can be responsible for large differences in their ability to balance and walk without issue.
In order to be on the lookout for increased fall risk in your loved one, you’ll need to pay careful attention to the medications that they take. You should reevaluate their medicine regimen in the nursing home. Many times, small adjustments or additions will be made once they enter a long-term care facility that may not be reflective of the medication they have taken in the past. These small changes can be responsible for large differences in their ability to balance and walk without issue.
Anti-Anxiety Drugs
One of the main culprits behind fall risk are anti-anxiety drugs. The general umbrella term for these is benzodiazepines, but you probably know them by their much more frequently used brand names: Valium (diazepam), Ativan (lorazepam), Restoril (temazepam), and Xanax (alprazolam). If your loved one is taking a drum that ends in -pam or -lam, it likely belongs to this family of anti-anxiety medications.
But why do anti-anxiety drugs cause falls to happen more often? It’s true that these medications can reduce anxiety and even help people to sleep, but this depressive function can change how a person’s neurons respond. In other words, their response times might not be ask quick as they were before. Recent studies have indicated that benzodiazepines (often simply abbreviates as “benzos”) may be associated with the development of dementia, and increased fall risk has been noted in patients who take them.
Among the medications used by those over the age of 65, benzodiazepines are highly common—as many as 8.7% of Americans over this age received a prescription. What they are not often told is that in addition to the fall-prone symptoms produced by the medicine, stopping these medications suddenly can also be dangerous. Dizziness, muscle tightness, anxiety, trouble concentrating, blurred vision, and unsteady legs are all symptoms that can occur from benzo withdrawal, and it’s not hard to see how these could lead to a fall injury. Thus, if a nursing home took your loved one off of their benzodiazepine prescription suddenly, a fall may be more likely.
Non-Benzo Sedatives
Benzodiazepines are not the only types of medication that can help to calm people. Non-benzo sedatives function as a calming agent, which can help with anxiety but are more often used to treat sleep disorders. These can arise naturally (e.g., an insomnia diagnosis), or they can happen as a consequence of getting older (confusion related to dementia, pain associated with arthritis keeping someone up, and so on).
Because these medications (which are sometimes called “Z-drugs”) are sedatives, they impair the ability to respond quickly on both a physical and mentally reactionary level. Imagine this as the difference between how skillfully you could complete a task when you are wide awake versus when you are struggling to keep your eyes open. Naturally, then, a person’s balance and ability to remain steady on their feet can be compromised.
Most commonly, your loved one will receive Ambien (zolpidem), Sonata (zaleplon), or Lunesta (eszopiclone) if they are taking sedatives. Some nursing homes find themselves in trouble for giving these medications to residents in an effort to make them easier to manage, and studies have shown that there is a positive correlation between being over the age of 65 and being given sedative drugs.
Antipsychotics
One of the most pressing issues that staff deal with in nursing homes is individuals who present behavioral difficulty. This is not necessarily the fault of the resident; they cannot control the manifestation of their dementia symptoms or the presence of schizophrenia or Alzheimer’s. That being said, many nursing homes will elect to place residents on an antipsychotic regimen to make them easier to attend to and speed up the nurses’ in-room tasks—a symptom of understaffing in nursing homes nationwide.
Be alert for common antipsychotics on your loved one’s list of medications. These include Risperdal (risperidone), Seroquel (quetiapine), Zyprexa (olanzapine), and Abilify (aripiprazole), among others. All of these medications are focused on treating types of psychosis, which can manifest as a lack of control over one’s behaviors. Such medicines help residents to regulate their moods and stay grounded, and those who have taken these medications for years may have adapted to the effect that the substances have on their bodies.
However, if your loved one is being newly prescribed an antipsychotic medication, they may be at an increased risk of falls. Some clinical research has found that certain types of antipsychotics (labeled “non-typical antipsychotics”) are closely related to hypotension, feelings of sedation, and even abnormalities in the way that people walk. As a result, the proportion of elderly individuals who have suffered fractures after a fall is higher in those who take antipsychotics than it is in the general population.
If your family member takes antipsychotics for an approved condition, the increased risk of falls may simply be something for which the nursing home must adjust its practices, given the benefit the patient receives. However, if the facility is simply prescribing antipsychotic medicine to make those with cognitive disabilities more tractable, this may not be an appropriate use case.
Anticonvulsants
At first glance, the term “anticonvulsant” can seem to be critically important—after all, if your loved one is convulsing, surely they should receive some sort of treatment. However, as with antipsychotics, many anticonvulsants are prescribed in nursing homes for the sole purpose of controlling and regulating “problematic” behaviors that make for more difficult interactions for staff. Most commonly, the purpose is to reduce the amount of time staff have to dedicate to each patient; in other words, residents are put on mood stabilizers so that staff can be in and out as fast as possible.
The two most common anticonvulsants that you’ll encounter are Depakote (valproic acid) and Neurontin (gabapentin). Many conditions benefit from the administration of these medications, so be aware of whether your loved one has been taking them for years or whether they are a part of a new medical plan when evaluating fall risk.
Clinical studies have drawn a strong correlation between the risk of falls and individuals taking anticonvulsants, because some of the symptoms they produce include blurred vision, dizziness, and ataxia, or poor muscle control that causes someone to be clumsy. Ataxia can manifest in a number of ways, from being unable to walk in a straight line to having difficulty pronouncing words or wrapping the fingers around something (like a cane or walker).
Compared to other age groups, geriatric patients are the number one demographic being prescribed anticonvulsant (or antiepileptic) medication, and this is even more problematic because of its impact on the bones. Antiepileptic medication reduces bone density—so should your loved one ever fall, the odds of breaking a bone are significantly higher.
If your loved one must taken an anticonvulsant due to a genuine medical condition like epilepsy (which can, itself, cause dangerous falls), medical professionals recommend gabapentin over other options in terms of reducing risk of falls as much as possible while still seeing a therapeutic benefit. However, the nursing home must take additional steps to mitigate fall risk if your family member is taking gabapentin.
Antidepressants
Unlike some of the previous medical interventions mentioned, antidepressants are chronically underprescribed in nursing homes; between 17% and 25% of patients in long-term care facilities battle with depressive symptoms but do not receive medicated treatment options. Despite this, those who are prescribed antidepressants must cope with an increased fall risk, as demonstrated by numerous studies.
However, the type of antidepressant at work here matters. Though they are less commonly prescribed in favor of more modern counterparts, tricyclic antidepressants (TCAs) have long been associated with an increased risk of falls in the elderly because one of their leading side effects is orthostatic hypotension—also called postural hypotension. This type of low blood pressure occurs when someone stands after sitting or lying down. Most people have experienced brief bouts of orthostatic hypertension, noticed as feeling lightheaded or the vision narrowing briefly when you first stand up. Naturally, this is a large contributor to falls in the elderly.
SSRIs, or selective serotonin reuptake inhibitors, are the primary class of antidepressants prescribed across America; you’ve likely seen these brand names often in the form of Zoloft (sertraline), Celexa (citalopram), Lexapro (escitalopram), Paxil (paroxetine), and Prozac (fluoxetine). SSRIs are heavily correlated with increased fall risk, especially in older women. Within the span of six months, at least 15% of women aged 65 and older will fall if they take antidepressants from the SSRI or TCA categories.
Other studies have indicated that the same risk is not as noticeably present with other types of antidepressants, such as SNRIs (selective norepinephrine reuptake inhibitors) with bupropion. The reason for this makes sense; bupropion does not affect how the body’s serotonergic system (that is, the body’s response to serotonin) works, and it is thought that something about how the body readjusts to less serotonin on SSRIs and TCAs makes it more difficult to maintain balance and clear vision.
However, the reduced incidence of falls in SNRIs and other less-used antidepressants is a correlation only. If your family member takes antidepressants, no matter the type, be vigilant for the possibility of increased falls and ensure that the nursing home takes precautions as well.
Opioid Analgesics
One of the defining features among medication usage in the older population is a consistent strategy to mitigate pain. Getting older can cause discomfort, whether from achy joints or other illnesses. In particular, opioid analgesics are commonly prescribed to elderly nursing home residents since they are highly effective in the treatment of substantial chronic pain.
If you’re unsure whether your loved one takes opioids, what you’re looking for is pain medicine that is more powerful than over-the-counter options like Advil. Instead, opioid analgesics are things like oxycodone/hydrocodone, methadone, codeine, morphine, and fentanyl.
In 2009, studies had not yet identified a strong association between taking opioid analgesics and a heightened risk of falls. However, a more recent study in 2020 was able to dive deeper into the data and reveal that this class of medications does in fact predispose patients to increased incidence of falls. In fact, the Centers for Disease Control have made a direct statement indicating that these narcotics be reevaluated “as part of fall risk management” when used therapeutically for nursing home residents.
But why would pain medicine be associated with falls? As with many of the other medications on this list, opioids can cause a sedative effect, and they are also associated with some level of cognitive impairment. In the studies analyzing their effect on falls, there was a correlation between not only whether residents took opioids but also at what dose—with higher doses associating with increased numbers of bone fractures related to falls.
Anticholinergics
You might expect that your loved one takes some pain medicine, maybe some sleeping medicine, and maybe even something for anxiety or depression. However, you might not think to check for anticholinergics, because these medications are prescribed for a wide variety of very different uses.
Anticholinergics block the body from seeing the effects of acetylcholine, which is a neurotransmitter. Acetylcholine is responsible for a lot of physical abilities as part of the nervous system, which is why anticholinergics can be so useful across a wide range of illnesses that have to do with how muscle and certain organs operate. Medications to look out for here include Benadryl (diphenhydramine), Phenergan (promethzine), Flexeril (cyclobenzaprine), Ditropan (oxybutynin), Detrol (tolterodine), Visatril (hydroxyzine), Scopace (scopolamine), and Antivert (meclizine).
Anticholinergics can be used to treat anything from bladder conditions and Parkinson’s disease to COPD (chronic obstructive pulmonary disease). While the therapeutic benefits of these medicines are often critical to a better quality of life for the elderly, it is important to remember that anticholinergics can function as sleep aids as well, bringing that same problematic sedative side effect that has been correlated with fall risk throughout the studies mentioned so far.
Antihypertensives
Finally, if there are still unidentified medications in your loved one’s regimen, they might be antihypertensives. Hypertension is the medical term for high blood pressure, so you may have simply heard of these medicines referred to in the past as “blood pressure meds.”
The good news is that whether or not hypertensive medications make your loved one more likely to fall will depend on how they specifically react to the medicine. Some people find themselves lightheaded or with a racing heartbeat when they take certain hypertensive medications; for this reason, studies are not able to definitively conclude that such medicine causes more falls.
Instead, be aware of how your loved one reacts to their blood pressure medication, and do not be afraid to push for different formulations if they show signs of lightheadedness, dizziness, or other concerning symptoms. According to some studies, around 90% of people above the age of 50 will develop high blood pressure, with 60% taking some sort of antihypertensive in response. Given how common this type of medication is, it’s critical that you help your family member advocate for themselves to keep them safe from falls.
Preventing Falls is the Legal Duty of the Nursing Home
Remember, even if your loved one has a higher fall risk due to medication, this does not mean it is acceptable for them to suffer falls. Nursing homes have a legal duty, under both state and federal law, to assess fall risk (including analyzing their medication regimen), and to implement reasonable fall preventative measures.
If a resident is a high fall risk due to the prescription drugs they take, this means the nursing home must do more to prevent them from falling.
Examples of fall preventative measures that can prevent harm include:
- bed alarms that ring when a resident gets up
- bed rails to keep a resident in bed
- maintaining a clutter free and well-lit environment
- lowered beds and floor mats to cushion for an inevitable fall
- toileting schedules to reduce the need to urinate in the middle of the night
- frequent 15 minute checks to ensure the resident is in their room and does not need assistance
- physician medication review to ensure the drugs being taken are not adversely impacting the resident’s balance or cognition
- non slip footwear like special socks
- keeping assistive devices like wheelchairs or walkers within reach
- sitters to provide 1 to 1 attention for times when a resident is having a bad day
Most of the above fall preventative measures are low cost, accessible, and oftentimes required by nursing home regulations.
Was My Parent’s Fall Preventable?
Unfortunately, in most of our facility fall cases that we handle, when we analyze the preventative measures used for a fall risk resident, they are usually lacking. This is a form of nursing home negligence.
If your loved one suffered a fall and injury inside a healthcare facility, visit this link to learn more about nursing home fall liability.
If you are ready to speak with our elder abuse and neglect law firm for your free case consultation, contact Senior Justice Law Firm by submitting your case facts below or calling us toll-free at 888-375-9998.


