Pressure Ulcer vs. Diabetic Ulcer
In a nursing home context, residents are often subject to wounds and injuries that are not typical of younger folks. This is often a result of a variety of factors, such as older age, less mobility, and even the potential for nursing home abuse and neglect. One of the most challenging avenues of wound diagnosis in long-term care facilities is the difference between pressure ulcers (sometimes called bedsores or decubitus ulcers) and diabetic ulcers.
While both types of skin lesions are visually similar and can even be caused by similar pathogeneses—or physical events that result in their development—they are two entirely separate types of injury, and nursing homes may have a vested interest in diagnosing a wound as a diabetic ulcer rather than a pressure ulcer. In order to understand why, it is critical to first know the difference between these injures, as well as what they mean for long-term care facilities.
Pressure ulcers and diabetic ulcers often get confused by medical professionals. It is nearly impossible to make the determination yourself as a layperson. Worse yet, sometimes a negligent nursing home will misdiagnosis a bed sore as a diabetic ulcer, to avoid liability. It is for this reason, if your loved one developed suspicious wounds during a nursing home residency or hospitalization, you should speak with an attorney immediately.
Free Case Consultation
Speak with a bed sore lawyer today by submitting your case facts below, live chatting with our office, or calling us at 888-375-9998. At Senior Justice Law Firm, nursing home negligence lawsuits are our law firm’s focus. This is all that we do. Let our lawyers help you on your journey to justice.
What Is a Pressure Ulcer?
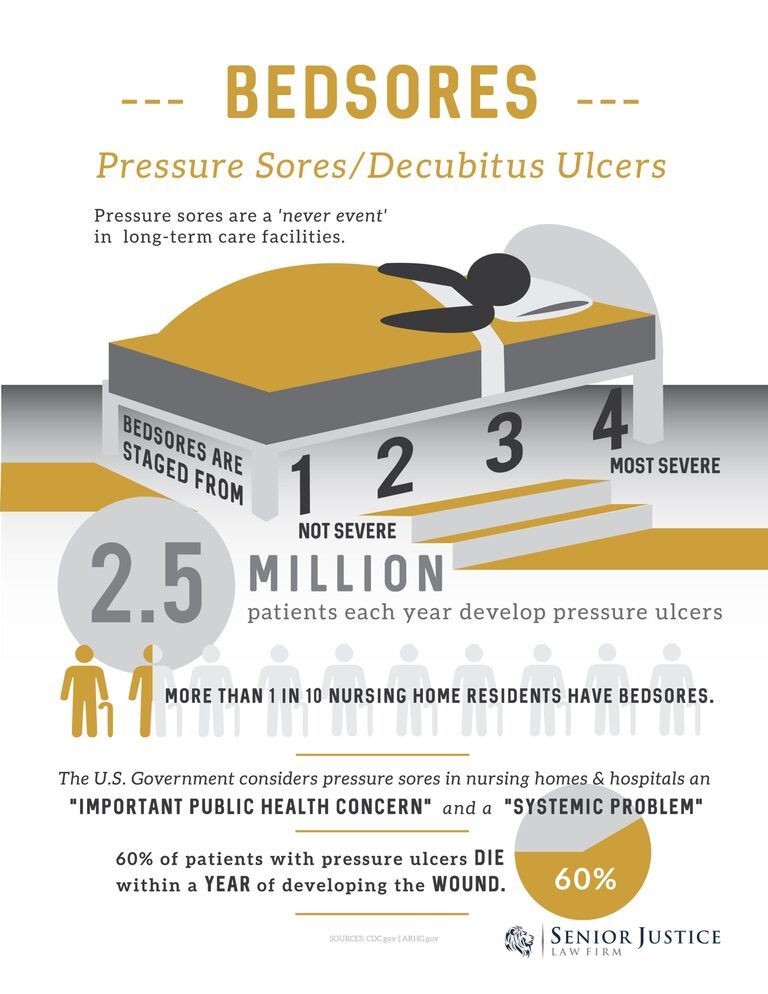
 A pressure ulcer is a type of skin lesion that results from reduced blood flow in areas that are under pressure, hence the name. Also referred to as bed sores, pressure ulcers are most common on the shoulders, elbows, and heels—the bony areas of the body where skin is thin.
A pressure ulcer is a type of skin lesion that results from reduced blood flow in areas that are under pressure, hence the name. Also referred to as bed sores, pressure ulcers are most common on the shoulders, elbows, and heels—the bony areas of the body where skin is thin.
Bedsores or pressure ulcers are a strong indicator of patient neglect. More often than not, the development of a pressure injury means the nursing staff failed to reposition the patient.
When the skin is placed under pressure, such as when the weight of the body is bearing down on an area, the blood vessels in the region are compressed. Blood flow slows, and the skin cells no longer receive the oxygen and nutrients that they need.
Once cells are deprived of oxygen, they begin to die, resulting in an open wound. If left untreated, a pressure ulcer will continue to worsen by expanding and progressing deeper into the flesh; severe decubiti can slough open until bone is visible as the surrounding tissue dies.
What Is a Diabetic Ulcer?
 Diabetic ulcers may look similar to pressure ulcers; however, it is important to note that they are not the same thing. As the name may imply, diabetic ulcers arise on individuals who have diabetes, and the foot is one of the most common areas affected by these skin sores.
Diabetic ulcers may look similar to pressure ulcers; however, it is important to note that they are not the same thing. As the name may imply, diabetic ulcers arise on individuals who have diabetes, and the foot is one of the most common areas affected by these skin sores.
Why do ulcers form on the skin of diabetes patients? In reality, many of the same players are at work in both pressure and diabetic ulcers. Diabetes causes neuropathy, or a dysfunction of the body’s nerves, most commonly at the periphery (or outer edges, such as the fingers and feet). When nerves are no longer functioning correctly, the body may no longer receive a signal that indicates pain when pressure is placed on an area for too long.
Similarly, consistently high blood sugar in diabetics can damage blood vessels, which reduces circulation. This combination of lower than average blood flow and lack of sensation are the starting points from which diabetic ulcers form.
Diabetic ulcers are a naturally occurring health condition. However, families must be wary of nursing homes trying to dress up a pressure injury as a diabetic ulcer.
Diabetic and Pressure Ulcer Confusion and Obfuscation in Nursing Homes
If a nursing home is managing a resident who is experiencing ulcers, the facility often has a direct interest in ensuring that the wound is not labeled as a pressure ulcer—and diabetic ulcers are a common scapegoat due to their similarities. Why would nursing homes become confused or inconsistent in their diagnosis of these two conditions?
One possible explanation is their similarity. Visually, the two types of ulcers can closely resemble each other, and especially in patients who do already have diabetes, the condition is a simple explanation for what may otherwise be the result of a complicated issue. However, even patients who are not diagnosed with diabetes may still be subject to having their wound identified as a diabetic ulcer. In order to determine what is true, medical staff will need to review the totality of the evidence, including whether the resident was lying down or exerting pressure on an area for an extended period of time.
Escaping Blame by Diagnosing a Pressure Injury as a Diabetic Ulcer
An additional—and unfortunately more common—reason that the two conditions are somewhat “interchangeable” is that residents with pressure ulcers represent a significant legal risk for nursing homes. Bedsores are almost entirely preventable. They form due to unrelieved pressure. Rarely will a disease or illness naturally cause them.
This means that pressure ulcers are a direct result of nursing home negligence in which staff failed to adequately assist residents in shifting their body weight (every two hours is recommended). When a nursing home is seeking to avoid a lawsuit due to pressure ulcers, one possible solution is to diagnose the skin lesion as a diabetic ulcer (which is not always preventable) instead.
Diagnosing a Bed Sore vs. Diabetic Wound
One of the most important means of determining whether a pressure ulcer is actually a diabetic ulcer is to look at its location. While diabetic patients can get pressure ulcers due to abuse or neglect in a nursing home, diabetic ulcers may appear in areas that are not typically subject to extended pressure—such as the bottoms of the feet when a resident has been lying down. In these cases, a diagnosis of a diabetic ulcer is more apt.
Receive a Free Attorney Consultation on Your Potential Diabetic vs. Pressure Ulcer Case
It is important to be aware that nursing homes may try to obfuscate the details of a skin wound to avoid the legal repercussions of diagnosing a resident with a pressure ulcer or bed sore. While diabetic ulcers may be a valid alternative diagnosis in some cases, some residents will be misdiagnosed in an effort to conceal a pattern of negligence and abuse by staff. Nursing homes with confirmed cases of bed sores may be fined, and consistent offenders could be added to the federal government’s list of long-term care facilities cited for confirmed abuse. Repeat issues at the same nursing home could see that location shut down permanently.
If you believe your loved one suffered a pressure sore in a health care facility, please contact the attorneys at Senior Justice Law Firm. We are here to help your family on your journey to justice. Call us toll free at 888-375-9998 or chat with us for free today.